It is the season of love – our thoughts are on chocolate covered strawberries and sweet delights, but that feeling in your stomach may be more than nervous flutters before your big date. Irritable bowel syndrome (IBS), a functional gastrointestinal disorder affecting up to ten percent of otherwise healthy individuals, is associated with a myriad of abdominal symptoms including pain, bloating, gas, and the urgency to have a bowel movement. IBS symptoms are at times worse (relapse) and other times are improved or gone (remitting). Many patients with IBS will also experience frequent variations in bowel movements ranging from diarrhea to constipation.
IBS is a chronic condition that must be managed symptomatically. Although sometimes debilitating, IBS is considered a functional ailment and not associated with adverse outcomes such as bowel obstruction, difficulty in the digestion or absorption of nutrients from food, or malignancy.
While anyone can be affected by IBS, symptoms occur most commonly in young adult women. Additionally, IBS is seen more frequently in the setting of psychological stressors such as anxiety and depression. While the cause of IBS is not completely understood, a growing body of evidence suggests the symptoms could stem from impaired communication between the brain and gut. Interestingly, the predominance of serotonin, a neuropeptide important in mood regulation, is synthesized and stored in the intestinal tissue (gut). While serotonin takes many forms and plays many roles, it is clear extensive communication occurs between the centers of the brain regulating stress response/mood and the gut. Additionally, research has shown the importance in balancing healthy verses unhealthy bacteria and organisms that occupy our intestinal tract. Finally, disturbances in the gut may contribute to leaky gut which leads to food sensitivities and additional abdominal symptoms.
Individuals with IBS symptoms may also have a long-standing history of abdominal issues abdominal cramping and bloating the most common complaints. Some individuals may also experience pain related to the passing of bowel movements. Urgency to have a bowel movement immediately after eating a meal can be very distressing socially and is a common trigger for a physician visit. These individuals report psychological distress if they are not near a restroom after eating. The urgency may also interfere with professional and social interactions.
Additionally, individuals with IBS may also have a long-standing history of diarrhea, often meal associated, and constipation requiring frequent laxative use. Many report fluctuation between diarrhea and constipation over time and changes of stool appearance, color, and mucous content. Evaluation of the patient presenting with IBS concerns includes a detailed history of symptoms, effect of dietary changes, and evaluation for warning signs that may suggest a more severe underlying condition. Patients experiencing unintentional weight loss, rectal bleeding, persistent vomiting, or who have a family history of inflammatory bowel disease may need additional evaluation or referral to a gastroenterology specialist.
It is important to differentiate irritable bowel syndrome (IBS) from Inflammatory Bowel Disease (IBD). While these two conditions sound similar, their symptoms and management are very different. Whereas IBS is a functional condition managed symptomatically, IBD is an autoimmune condition requiring aggressive management by a gastroenterologist. If not managed effectively, IBD is associated with severe bowel disease including obstruction, strictures, and perforation of the bowel which may lead to serious injury or death. Additionally, patients and families with a history of inflammatory bowel disease may require more aggressive screening for colon cancer. A discussion with your primary care physician can identify if your symptoms are consistent with irritable bowel syndrome or if further evaluation for inflammatory bowel disease is warranted.
There is no specific laboratory test or imaging study needed for a diagnosis of irritable bowel syndrome, however your physician will take a history and perform a physical examination. An empathetic approach to care is needed for patients with IBS as these symptoms can be very debilitating. The initial approach to symptom management may focus on reduction of stress and dietary changes. Highly processed foods found in fast food restaurants and convenience items must be eliminated from the diet. A high fiber diet is usually recommended with a focus on whole grains, fruits, and vegetables. Highly processed fats and oils should also be reduced/avoided. Some physicians may prescribe a food elimination diet or perform specialized testing for food sensitivities. Referral to a nutritionist/dietician may also be helpful in dietary management of symptoms.
While medication is not routinely recommended for irritable bowel syndrome, for patients with symptoms that are difficult to treat or manage, artificial fiber, antispasmodics, and serotonergic medications may be prescribed.
Healthy diet, good sleep, and regular exercise go a long way in promoting optimal gut health and preventing/reducing functional conditions such as irritable bowel syndrome. If you experience persistent or worsening abdominal symptoms, talk to your physician. Your physician will determine if an additional evaluation is needed and provide insight into dietary changes or treatments appropriate for you.
Kendall Wagner, M.D. is a regular healthcare contributor to Do South Magazine.
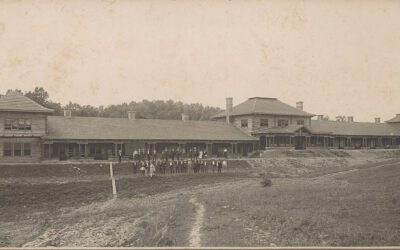
Chaffee Crossing Clinic
11300 Roberts Boulevard, Fort Smith, Arkansas
479.242.5910
chaffeecrossingclinic.com