The days are quietly getting longer and the frost a little lighter in the mornings as small bits of green grass can be seen peeking through the dull brown carpet covering our lawns. Spring will be here soon! While we welcome the burst of color and life that spring brings, many of us will soon be sneezing, rubbing our eyes, and clearing our throats. According to the American College of Allergy and Immunology, allergies are the sixth leading cause of chronic disease in the U.S. with an estimated fifty million Americans suffering from allergies each year. In fact, the estimated economic impact of allergies exceeds eighteen billion dollars per year!
Allergies as a disease can be divided into seasonal and perennial. Seasonal allergy sufferers usually experience symptoms in spring, summer, and early fall. These symptoms are usually triggered by allergic sensitivity to pollens from grasses, trees, and weeds, or may also be triggered by airborne mold spores. Perennial allergy sufferers experience symptoms year round and usually are sensitive to more insidious stimuli such as dust mites, animal dander, cockroaches, and mold spores.
Allergic rhinitis, sometimes referred to as “hay fever,” presents with a constellation of symptoms including stuffy or runny nose, sneezing, watering of the eyes, and a sensation of itchiness of the eyes, nose, or roof of the mouth. Contrary to the common name, allergic rhinitis is very rarely associated with fever. It is important to distinguish these acute symptoms from sinusitis or a sinus infection that is usually characterized by symptoms lasting longer than ten days, facial pain/pressure, and fever greater than 101° Fahrenheit. Many people mistake the presence of purulent (discolored) nasal discharge as an indication of sinus infection, but this finding simply indicates the presence of white blood cells in the nasal discharge, and may be seen in allergic, viral, and bacterial causes of nasal discharge lasting longer than a couple of days.
Treatment of allergic rhinitis usually does not require the use of antibiotics. That is why it is important to distinguish between allergic rhinitis and sinusitis. With more antibiotic resistance developing, it is important to use antibiotic treatment only when necessary! Thankfully, treatment of allergic rhinitis can often occur without a physician office visit. Many of the basic medications are available over the counter. Early treatment with over the counter (OTC) medications can prevent progression of allergic rhinitis into sinusitis further reducing the need for antibiotics.
OTC medications available for the treatment of allergies include antihistamines such as Zyrtec (Cetirizine), Claritin (Loratadine), and Allegra (Fexofenadine). These medications work by blocking the release of histamine, a protein involved in triggering an inflammatory cascade that results in the symptoms referenced above. While these medications are generally safe in most patients from infancy through elder years, it is important to always talk to your doctor and pharmacist about other medications you may be taking and potential side effects of these medications. Benadryl (diphenhydramine) has also been used historically for the treatment of allergy symptoms but can have unwanted side effects such as sedation (sleepiness) and grogginess/confusion (brain fog) in some patients and should be used with caution. Topical medications such as Flonase (Fluticasone) nasal spray or Astelin (Azelastine) may be used for isolated nasal stuffiness or runny nose, while Patanol (Olopatadine) eye drops may be used for isolated symptoms of itchy and watery eyes. Your physician may even recommend a combination of oral medication, nasal spray, and eye drops to effectively treat your symptoms.
Longer term solutions in the management of allergic disease include avoidance of the allergic trigger (avoiding outdoors during peak pollen times), decreasing the exposure to the trigger (special pillowcases/mattress covers for dust mites), chronically prescribed allergy medications, and finally allergy immunotherapy. All these treatments may be used at different times in the management of a patient with allergies. Usually, these treatments may be preceded or guided by allergy testing. Allergy testing can be performed by your doctor or an allergist (specially trained physician who focuses on treatment of allergic disease). In your primary doctor’s office, testing may consist of a blood test, while an allergist usually performs skin-prick testing that has been viewed as the gold standard in identifying allergic triggers. Such testing may be used to formulate an allergy immunotherapy plan (i.e. allergy shots) usually under the direction of an allergist or specially trained physician.
As spring arrives, know that you do not suffer alone and there are great treatment options available for both seasonal and perennial allergic disease. Many of these treatments are available at your hometown pharmacy! Call your physician’s office today to schedule a consultation about management of allergic rhinitis. Remember, do not start any new medication regimen without first consulting with your physician and pharmacist!
Kendall Wagner, M.D. is a regular healthcare contributor to Do South® Magazine.
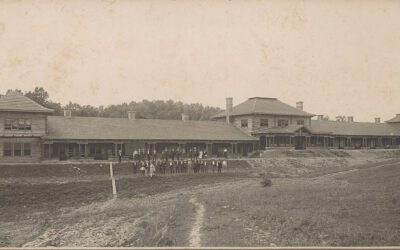
Chaffee Crossing Clinic
11300 Roberts Boulevard, Fort Smith, Arkansas
479.242.5910
chaffeecrossingclinic.com